Carpal Tunnel Syndrome (CTS)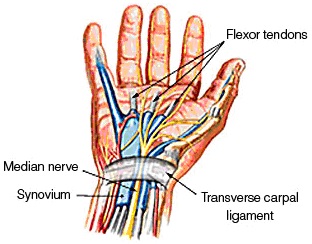
- The most common nerve compression is the median nerve as it passes through the carpal tunnel, ‘Carpal Tunnel Syndrome’ (the carpal tunnel is the space formed by the carpal bones and the transverse carpal ligament, and carries the flexor tendons and median nerve from the forearm into the hand)
- CTS is typically worse at night (this could be due to wrist flexion posture when sleeping and/or relative peripheral fluid retention associated with reduced blood pressure when sleeping) and is associated with pins & needles /numbness in the index, middle fingers, 1/2 ring finger and thumb. Pain and clumsiness also associated with CTS
- Conservative management involves splinting the wrist in neutral for sleeping, and also for other activities that provoke symptoms
- Clinical tests include Tinel’s sign (tapping from mid-palm, proximally over wrist which reproduces tingling or shooting sensations), Phalen’s test (wrist flexed for up to 1 minute reproduces tingling in fingers)
- Nerve conduction studies can be helpful in confirming CTS and the degree of severity (mild, moderate or severe)
- Mild to moderate CTS is more likely to respond to splinting
- Thenar muscle wasting or weakness in palmar abduction indicates more severe nerve compression, with surgical release the most appropriate treatment. Motor recovery may not return if nerve compression severe or prolonged
Pronator Syndrome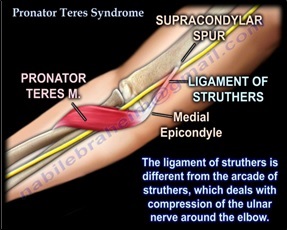
- Compression of the median nerve at the elbow
- 5 sites of entrapment – supracondylar process, Ligament of Struthers, bicipital aponeurosis, between ulnar & humeral heads of pronator teres, or FDS aponeurotic arch
- Presents with parasthesia in radial half of hand, often made worse with repetitive pronation/supination activity
- Not associated with night symptoms
- Clinical tests include positive Tinels sign proximal anterior forearm but negative at wrist. Negative Phalen’s test
- Resisted elbow flexion with forearm supination for compression at bicipital aponeurosis
- Resisted pronation with elbow extended for compression at two heads of pronator teres
- Resisted contraction of FDS to middle finger for compression FDS fibrous arch
- Conservative management includes rest, splinting (to control forearm rotation), activity modification and is suitable for mild to moderate symptoms
- Commonly associated with medial epicondylagia
Anterior Interosseous Nerve Syndrome
- Terminal motor branch of median nerve and arises just distal to medial epicondyle and supplies FDP (index & middle), FPL and pronator quadratus
- Presents without pain or parasthesia, but weakness of grip and inability to make OK sign. Pronation weak on resisted testing with elbow maximally flexed
- Possible entrapment sites: tendinous edge of deep head pronator teres, FDS arcade, accessory head FPL
- Distinguish from FPL rupture by passively moving wrist back and watch for thumb tip bend
- May be associated with viral brachial neuritis
- Treatment may involve elbow splinting at 90˚ flexion (for 8 -12 weeks), or surgical decompression
References:
McKean J (2014), Carpal Tunnel Syndrome, www.orthobullets.com;
Abbasi D (2014) Pronator Syndrome, www.orthobullets.com,
Nabil E (2014) Pronator Teres Syndrome – Everything you need to know, www.youtube.com/watch?v=ZqhO1dzqTtY ;
Vitale M (2014), AIN Compressive Neuropathy, www.orthobullets.com




