MANAGEMENT OF PAEDIATRIC HAND FRACTURES
The composition and biomechanical properties of paediatric bone differs to that of an adult, therefore resulting in different fracture patterns, healing processes and overall management. Paediatric bone is less dense, has a lower mineral content and is more elastic giving it a greater tolerance to bending forces than adult bone. Due to having a thick and extremely osteogenic periosteum, bone healing is more rapid and predictable in children than it is in adults.
For children 0-6 years, most hand fractures tend to occur within the home environment and involve a crush injury to the distal phalanx of the fingers or thumb. In the 6-14 year age group there is more of a tendency for fractures to occur outside of the home environment during outdoor play or sporting activities and most commonly involve the proximal phalanx of the little finger or the metacarpal of the thumb or little finger.
Fractures involving the growth plates are unique to children and recognising the common paediatric fracture locations and patterns is essential in ensuring prompt and appropriate treatment. If correctly diagnosed and managed, excellent clinical outcomes can be achieved and complications with skeletal growth and development avoided.
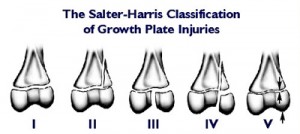
Salter Harris Classification System: This classification divides fractures into five types based on whether a fracture involves the metaphysis, physis or epiphysis.
- Type 1: Fracture through the physeal plate (often not detected radiographically)
- Type 2: Fracture through the metaphysis and physis (most common; up to 75% of all physeal fractures)
- Type 3: Fracture through the epiphysis and physis
- Type 4: Fracture through the metaphysis, physis and epiphysis
- Type 5: Crush injury involving part or all of the physis (Tend to arrest bone growth and in almost all cases requires surgery)
Regardless of whether the growth plate is involved or not, paediatric hand fractures are best reviewed by a Hand Surgeon (orthopaedic or plastic surgeon who specialises in injuries of the hand and upper limb) and Hand Therapist to ensure the most appropriate management option is selected.
Most paediatric fractures are managed non-operatively, however if there are concerns regarding bony alignment or rotation/angulation of the finger is observed, surgical intervention may be required. The aim of restoring bony alignment is to ensure the fracture does not impede joint movement and hand function once healed.
All paediatric fractures, should be immobilised in a splint or cast for a period of up to 3-6 weeks to allow undisturbed healing and to avoid bony displacement. In most cases buddy taping alone is not sufficient and if done incorrectly, can worsen angulation or rotation by holding a displaced fracture in incorrect alignment. The position of the wrist, fingers and thumb in the cast or splint as well as what joints are included, varies depending on the location of the fracture.
Following the necessary period of immobilisation, which varies depending on the child’s age and the severity of the injury, hand therapy commences to restore movement and strength and a graded return to pre-morbid function takes place.
References:
Al-Qattan, M., Hashem, M., Rasool, A., Eshayeb, J., & Hassanain, J. (2004) A unique fracture pattern of the proximal phalanx in children: fractures through the phalangeal neck with an attached dorsal bony flange. Injury-international Journal of The Care of The Injured, 35, 1185-1191
Gupta, A. Kay, S. Schecker, L. (2000). The growing hand. San Diego, CA: Harcourt Brace
Hovius, S. Foucher, G. Raimondi, P. (2002). The Paediatric Upper Limb. London: Martin Dunitz
Nellans, K., & Chung, K. (2013) Paediatric hand fractures. Hand Clinics, 29(4), 569-578
Sivit, A., DuPont, E., & Sivit, C. (2013) Paediatric hand injuries; essentials you need to know. Emergency Radiology, 21, 197-206.
Vadivelu, R., Dias, J., Burke, F., & Stanton, J. (2006) Hand Injuries in Children. Journal of Pediatric Orthopedics, 26(1), 29-35
Young, K., Greenwood, A., MacQuillan, A., Lee, S., & Wilson, S. (2013) Paediatric hand fractures. Journal of Hand Surgery, 38(8), 898-902