Rehab following an Extensor tendon repair requires wearing a splint, frequent specific exercises, activity modification, and adherence to precautions to ensure you get the best outcome from your surgical repair and optimal return of movement and function in the affected hand.
A tendon heals slowly, it will initially weaken after surgery, then get stronger gradually, with full healing after three months.
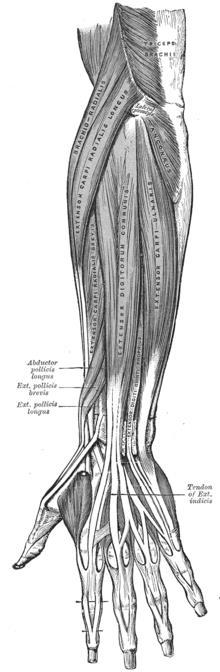
Fingers: The extensor tendons from the forearm muscles are used to straighten the knuckles, and a complex mix of those tendons and muscles within the hand straighten the finger joints. There is one muscle that divides into four tendons to each finger called Extensor Digitorum Communis (EDC), and the little and index fingers also have their own extensor muscles (Extensor Digiti Minimi – EDM & Extensor Indicis Proprius – EIP).
Thumb: The thumb extensor muscles lie in the forearm, and the most common to be lacerated is the one that goes past the end joint and straightens it; it is called the Extensor Pollicis Longus (EPL).
Rupture Rupturing of the repaired tendon can occur from using the hand before the repair is strong enough, over exercising, scar adhesions. There may be a loss of movement, or you may experience a springing feeling when the tendon ruptures. A ruptured tendon can sometimes be repaired, but to get the best outcome it is essential to care for the first repair. The tendon is repaired with fine stitches that can be pulled apart if not protected appropriately post repair.
Important precautions are:
• Finger repair: Do not use the fingers for any activity – even the unaffected
fingers. The thumb may be used freely.
• Thumb repair: Do not use the thumb for any activity. The fingers may be used freely.
• Splint is worn 24 hours per day. Keep on for showers, sleeping, dressing etc.
• Only complete the exercises as practiced in therapy. Doing more or less can increase the chance of rupture. The exercises will be changed to compliment the healing stage of the tendon.
• Do not play contact sports, or any activity if there is a risk of falling, or drive.
Therapy will include:
• Education
• Splinting
• Wound management
• Scar management
• Oedema management
• Exercise
• Activity modification
• Strengthening

